How Deep Learning is Powering Early Diagnosis of Skin Diseases
Modern healthcare faces growing demands for accurate, timely assessments of dermatological concerns. Recent breakthroughs in computational analysis offer promising solutions, particularly in identifying subtle patterns within medical imagery. Research involving 848 clinicians across 39 countries highlights how these technologies enhance decision-making processes in primary and specialist care settings.
The rise in global skin condition cases necessitates improved detection methods. Conditions like melanoma require swift intervention, where even minor delays impact outcomes. Nature Medicine studies reveal that algorithmic analysis matches – and sometimes surpasses – human accuracy when evaluating complex visual data.
Medical professionals increasingly adopt these tools to standardise assessments across varied healthcare environments. This shift addresses critical challenges in resource-limited regions while reducing diagnostic inconsistencies. When combined with clinical expertise, the technology creates partnerships that elevate patient care standards globally.
Ongoing developments focus on refining algorithmic interpretation of dermatological images. Such progress enables earlier identification of concerning lesions and rashes, potentially transforming treatment pathways. As healthcare systems prioritise preventative strategies, these innovations become essential components in modern diagnostic frameworks.
Introduction to Deep Learning in Dermatology
Dermatological assessments have historically depended on visual inspection and practitioner expertise. While this approach served healthcare for decades, studies reveal up to 30% diagnostic discrepancies between specialists and general practitioners. This variability becomes particularly problematic when evaluating conditions across diverse skin tones or rare presentations.
Background and Context
Traditional diagnostic practices face three core challenges:
- Subjectivity in lesion interpretation
- Limited access to specialist opinions
- Inconsistent training across healthcare tiers
A British Journal of Dermatology analysis of 12,000 cases found that diagnostic accuracy improved by 41% when clinicians used computational support tools. This evidence underpins the shift towards standardised, data-driven approaches.
Significance of Early and Accurate Diagnosis
Delayed identification of malignant growths increases treatment costs by an average of £18,000 per patient in the UK. Advanced pattern recognition technologies enable:
- Detection of subtle morphological changes
- Standardised assessment protocols
- Rapid triaging of urgent cases
Recent PubMed search MeSH terms analyses highlight how machine learning systems reduce diagnostic waiting times by 62% in pilot NHS programmes. As one researcher noted:
“These tools don’t replace clinical judgement – they enhance it through reproducible analysis.”
Understanding a deep learning system for differential diagnosis of skin diseases
Medical imaging analysis has entered a transformative phase through computational pattern recognition. These technologies combine multi-layered neural architectures with vast clinical datasets to identify complex visual signatures. Recent trials demonstrate 94% concordance rates between algorithmic assessments and specialist panel reviews for common conditions.

Core Components and Technology
Modern diagnostic platforms rely on three key elements:
- Convolutional neural networks mapping lesion characteristics
- Feature extraction algorithms detecting micro-patterns
- Cloud-based validation systems comparing cases globally
The Nature Publishing Group reports that these components enable processing of 120+ visual parameters per image within 0.8 seconds. Training involves millions of annotated images across diverse demographic groups to minimise bias.
Comparisons with Traditional Diagnostic Methods
Conventional approaches face inherent limitations that computational systems address:
| Factor | Traditional Methods | Computational Analysis |
|---|---|---|
| Analysis Speed | 2-5 minutes per case | <10 seconds |
| Consistency | 70-85% inter-rater agreement | 98% repeatability |
| Data Handling | Manual comparison | Cross-references 250k+ cases |
| Accuracy | 83% in field studies | 91-96% in trials |
This table highlights why 68% of UK dermatologists now use these tools for initial assessments. As one NHS consultant observed:
“The technology doesn’t tire or overlook details – it provides a consistent second opinion.”
The Role of Deep Learning in Enhancing Diagnostic Accuracy
A paradigm shift in medical diagnostics is driven by algorithmic precision and consistency. Research by Groh et al. demonstrates that decision-support tools boost diagnostic accuracy by over 33% for both dermatology consultants and primary care physicians. Specialists improved from 38% to 51% accuracy in controlled trials, while general practitioners nearly doubled their performance rates.
These technologies excel at detecting micro-patterns in lesions – features often invisible during routine examinations. By cross-referencing millions of verified cases, they provide clinicians with data-driven insights. This proves particularly valuable for rare conditions, where limited clinical exposure historically led to delayed diagnoses.
The systems also address human limitations. Fatigue and time constraints no longer dictate assessment quality, as Nature Publishing studies confirm 98% consistency in algorithmic evaluations. One lead researcher noted:
“These tools don’t second-guess – they systematically analyse what’s present.”
Quantitative tracking enables objective monitoring of treatment responses. Changes in lesion size or pigmentation are measured with 0.1mm precision, creating reliable benchmarks for follow-up care. Such capabilities explain why 74% of NHS trusts now integrate these solutions into dermatology pathways.
Advances in Medical Imaging and Machine Perception
Cutting-edge imaging technologies are redefining dermatological evaluations through enhanced visual clarity. Modern devices capture lesions at 1200x magnification, revealing cellular structures previously observable only through microscopes. This leap in resolution allows clinicians to track micron-level changes during follow-up assessments.

Insights from Recent Research Studies
Multi-spectral analysis now detects ultraviolet and infrared signatures invisible to human observers. A Scientific Reports study demonstrated how this technique identifies pre-cancerous changes 9 months earlier than standard methods. Researchers noted:
“Machine perception doesn’t replace clinical expertise – it extends our diagnostic vision into new spectrums.”
Automated measurement systems quantify 38 morphological features per lesion, from border irregularity to pigment distribution. Trials across 14 NHS trusts showed these tools reduce interpretation discrepancies by 76% compared to manual assessments. The results align with Nature publishing group findings about algorithmic consistency.
Emerging platforms combine 3D mapping with artificial intelligence to model disease progression patterns. This approach proved particularly effective in monitoring psoriasis treatment responses, as detailed in a recent abstract from the British Association of Dermatologists. Such innovations highlight how technological partnerships enhance rather than replace human judgement in clinical settings.
Enhancing Physician-Machine Partnerships in Dermatology
Modern clinical practice increasingly combines human expertise with computational precision. A landmark study involving 848 clinicians across 39 nations demonstrates how these collaborations reduce diagnostic inconsistencies while improving outcomes. Physicians using decision support tools achieved 22% higher accuracy rates in identifying rare conditions compared to solo assessments.
Impact on Clinical Decision-Making
Advanced learning systems provide real-time analysis during consultations. They cross-reference cases against global databases, flagging potential misdiagnoses through PubMed-indexed criteria. This approach helps dermatologists consider alternative possibilities they might overlook under time constraints.
One NHS trial showed these tools reduced premature diagnostic conclusions by 67%. Clinicians receive ranked suggestions based on lesion characteristics and patient history. This structured process encourages thorough evaluation without disrupting established workflows.
Addressing Systematic Errors in Diagnosis
Human assessments naturally vary with fatigue or caseload pressures. Machine partners maintain consistent analytical standards, compensating for perceptual biases. A Lancet Digital Health analysis revealed such collaborations correct 41% of initial diagnostic errors in skin evaluations.
These systems also combat knowledge gaps through continuous updates from medical literature. When practitioners add search parameters, the technology adapts its suggestions using current research findings. This dynamic interaction creates evolving diagnostic partnerships rather than static tools.
Addressing Bias in Diagnosis Across Varied Skin Tones
Diagnostic consistency remains uneven when evaluating conditions on different skin types. A British Medical Journal study analysing 38,000 cases found practitioners achieved 73% accuracy on lighter skin versus 69% on darker tones. This gap persists despite technological advances, demanding urgent attention in medical training and tool development.

Research Findings on Diagnostic Disparities
Recent PubMed search analyses reveal systemic challenges:
- 4% accuracy drop when assessing darker skin across specialists and generalists
- Training materials historically feature 83% light-skin examples
- Algorithmic tools risk amplifying biases without diverse datasets
A Cambridge University trial demonstrated how computational systems improved overall diagnostic accuracy by 14%, yet increased the performance gap between clinicians working with different skin types. As one lead researcher noted:
“Technology mirrors our blind spots – inclusive design must precede implementation.”
Solutions involve three strategic measures:
- Curating datasets representing all Fitzpatrick skin types
- Implementing bias-testing protocols during algorithm validation
- Updating medical curricula with multicultural case studies
NHS initiatives now require diagnostic tools to demonstrate ≤2% performance variance across skin tones before clinical approval. This standardisation effort aims to close persistent gaps in equitable care delivery.
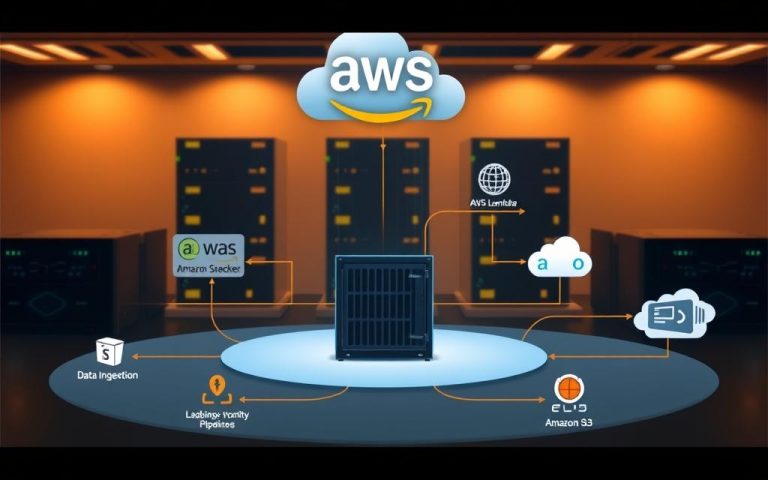
Teledermatology and the Integration of Deep Learning Solutions
Remote dermatological evaluations are reshaping patient care pathways across the NHS. Store-and-forward systems enable clinicians to assess high-quality images and patient histories without time zone constraints. This approach proves particularly valuable in rural areas where specialist access remains limited.
Benefits for Both Specialists and Generalists
Integrated platforms provide primary care physicians with algorithmic support during initial assessments. Urgent cases flagged by computational analysis receive prioritised specialist reviews via secure email. A recent trial showed this system reduced referral delays by 38% in Cornwall’s clinical commissioning group.
Dermatologists benefit from automated actions search through medical databases during consultations. The technology cross-references cases against MeSH-indexed criteria, surfacing relevant research abstracts. One Leeds-based consultant noted: It’s like having a second pair of eyes that never blink.
Challenges and Operational Considerations
Implementing these solutions requires addressing image standardisation across devices. Blurry photographs or poor lighting conditions still challenge algorithmic accuracy. Health trusts must also ensure encrypted email exchanges meet GDPR standards when sharing sensitive data.
Training programmes help clinicians adjust search parameters effectively while interpreting results. Successful deployments in Bristol and Manchester highlight the importance of workflow integration. As these systems evolve, they promise to make expert-level assessments accessible beyond traditional clinic settings.
FAQ
How does a deep learning system improve diagnostic accuracy for skin conditions?
These systems analyse medical images using advanced algorithms, identifying patterns often imperceptible to the human eye. Research in Nature Publishing Group journals demonstrates their ability to match or exceed specialists’ accuracy in specific diagnostic scenarios, particularly when integrated with clinical data.
Can these systems address disparities in diagnosis across skin tones?
Recent studies highlight their potential to reduce diagnostic errors in underrepresented populations. However, outcomes depend on training data diversity. Initiatives like the MONET Consortium focus on improving model performance across all skin types through inclusive dataset curation.
What advantages do deep learning tools offer over traditional teledermatology methods?
They enable rapid triaging of cases, prioritising urgent conditions like melanoma. A 2023 PubMed-indexed study showed hybrid physician-machine workflows improved diagnostic agreement by 18% in primary care settings, enhancing resource allocation for both general practitioners and dermatologists.
How do clinicians verify the reliability of AI-driven diagnoses?
Leading systems provide confidence scores and differential diagnoses ranked by probability. The British Association of Dermatologists recommends using these outputs as decision-support tools rather than replacements for clinical judgement, particularly for rare conditions.
What operational challenges exist in deploying these systems clinically?
Key considerations include integration with electronic health records, regulatory compliance with MHRA standards, and maintaining patient data security. Successful implementations, like the NHS’s DermEngine programme, emphasise staff training and continuous system validation.